![]() The Pacific War Online Encyclopedia
The Pacific War Online Encyclopedia
|
| Previous: Medford | Table of Contents | Next: Medium Bombers |
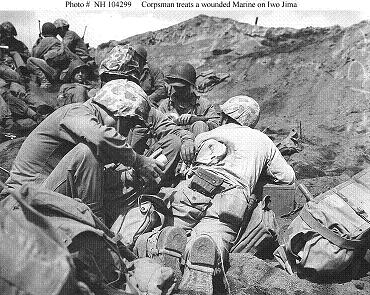
Naval
History
and Heritage Command #NH 104299
The Second World War saw tremendous improvements in medical care
for casualties. For
example, in the U.S.
Army, the death rate among
wounded men was 4.5% versus 8.1% in the First World War. Much of
this
progress came from the use of new drugs, such as antibiotics, and
the
widespread use of transfusions of both whole blood and plasma. The
greater speed with which wounded men could be evacuated to a
hospital
was equally important. There were far more motor vehicles on the
battlefield than in the First World War, and air evacuation of
casualties became increasingly commonplace, particularly in the
Pacific. In addition, the aid stations and hospitals themselves
were
situated closer to the front line.
There seems to be wide agreement that the general operative surgery of our Second World War has not been materially more advanced or more skillful than that of our previous war. The more brilliant results have been accomplished by bringing that surgery closer to the casualty both in time and distance. And new factors have aided in these results, the routine transfusion of plasma, albumen and whole blood, the use of sulfonamides and penicillin and air evacuation of casualties.
(Quoted in Cowdrey 1994.)
It was fortunate that medical care had so improved, because the Pacific was an extremely unhealthy place. Along with the obvious hazards of combat, soldiers in the Pacific faced the dangers of malaria, dengue fever, and other tropical diseases, which were transmitted by mosquitoes and other arthropods. Contaminated water could cripple combat units with various forms of dysentery. So could poor field sanitation. In an environment swarming with exotic microbes, even slight wounds stood a good chance of rapidly becoming infected. The wet climate meant that clothing, and particularly footwear, were waterlogged for long periods of time, which encouraged trench foot and the fungal infections known as "jungle rot."
Wounds. Treatment of wounds was directed at reversing the effects of blood loss, preventing infection, and repairing damage. Massive blood loss could kill a man within minutes and had to be controlled at once by the front-line medic. This often meant the use of tourniquets. Great faith was placed by the Allies in the newly developed dried plasma kit, which consisted of two cans containing a bottle of 400 cc (not quite a pint) of distilled water and a bottle of dried plasma. The water was added to the plasma, which was ready to infuse into a patient in three minutes. Unlike whole blood, the dried plasma had a long shelf life and did not have to be matched to the blood type of the patient.

National Archives. Via Steinert (2000)
Plasma undoubtedly saved many men who would
otherwise have perished from blood loss, but it became
increasingly
clear that it could not always stave off shock, a
condition that put a man in a rapid downward spiral towards death.
Shock resulted from lack of oxygenation of the body's tissues,
and,
while plasma could maintain the circulation of the blood, it did
not
contain the red blood cells responsible for carrying oxygen to the
tissues. By 1943 it was recognized that there was no substitute
for
whole blood for treating shock, and the Allies put together an
impressive system of blood banks to ensure that the
necessary
blood got to the field hospitals. "Plasma and albumin work wonders
on
wounded men," one medic observed, "but whole blood is life itself"
(Cowdrey 1994).
Wound infection was controlled surgically as well as with drugs. The basic prevention for gangrene was then, as it remains today, thorough debridement of the wound. Debridement is the surgical removal of all dead and dying tissue from the wound, leaving only healthy tissue, which has considerable resistance to infection. This required the surgeon at the field hospital to completely open the wound in order to get at all the damaged flesh. The wound was then dressed but left unsutured until the patient reached a rear area hospital, where it was sutured only once there was confidence that no dead tissue had been missed. Surgical repair of wounds was also left to the rear area hospitals.
The most serious form of wound infection was gas gangrene, caused by anaerobic bacteria multiplying in dead muscle tissue and producing bubbles of foul gases as well as powerful toxins that killed surrounding tissue. Severe cases could be controlled only by amputation, which sometimes was more than the debilitated patient could survive. Debriding and leaving the wound open to the air (oxygen being toxic to anaerobic bacteria) helped prevent gas gangrene, as did treatment with gas gangrene antitoxin, which helped prevent its spread.
Another dreaded form of wound infection was
tetanus, also caused by anaerobic bacteria closely related to
those
responsible for gas gangrene. Tetanus does not spread like gas
gangrene, but it produces a potent nerve toxin that causes every
muscle
in the body to go rigid, causing the patient incredible suffering
and
leading to death from exhaustion or suffocation. However, tetanus
is
easily vaccinated against using a deactivated form of its toxin,
and
every American soldier was so vaccinated on induction. As a
result, the
U.S. Army recorded only 12 tetanus cases, out of 3,000,000
hospital
admissions for wounds or injury, during the entire war.
Among the new drugs available in 1941 for helping
to control wound infections were the sulfa drugs, which were
derived
from aniline dyes. They got their name from the sulfonamide group
that
gave the drugs their antibacterial properties. These drugs stopped
the
multiplication of bacteria by a mechanism not then understood,
which
allowed the body's defenses to overcome bacterial infections. The
sulfa
drugs created a sensation, in spite of hazards such as allergic
reactions in some patients and crystallization in the kidneys of
others
(causing intense pain). American soldiers carried a supply
of
sulfanilamide powder as part of their field kit, which was to be
sprinkled in any open wound, and medics carried sulfa tablets to
be
swallowed. The sulfa drugs undoubtedly saved countless men from
serious
wound infections. Sulfapyridine, also known as M&B 693, was
widely
used to cure pneumonia.
Penicillin was still in the experimental stage in 1941, when British researchers came to the United States to seek assistance in its mass production. This was accomplished in 1943 by finding a strain of Penicillium chrysogenum on a moldy cantaloupe in Peoria, Illinois, that produced large quantities of the drug when grown in corn steep liquor using deep-tank fermentation. The first doses (1000 ampules of 100,000 units each) reached the South Pacific in October 1943. Production soared (exceeding 7 trillion units in 1945) and all restrictions on its use were dropped in March 1944. Penicillin was even more effective than sulfa drugs against gram-positive bacteria, actually killing the microorganisms both in the laboratory and in the human body, rather than merely inhibiting their multiplication. Unlike almost all other antibacterials of the day, including the sulfa drugs, it was almost completely nontoxic, though allergic reactions were seen in a few individuals.
The new antibiotics became a crutch for some physicians, who became careless about thorough debridement through a mistaken belief that antibiotics made this unnecessary. Antibiotics could not reach dead tissue in deep wounds and physicians soon learned that thorough debridement was still necessary. However, the combination of proper debridement and antibiotics was more effective than debridement alone.
When only primitive medical care was available, as in Japanese prisoner of war
camps, it was not unknown to use maggot therapy to debride wounds.
Insect larvae would be deliberately introduced into the wound and
would
consume necrotic tissue, leaving healthy tissue largely untouched.
The
technique had been used in controlled medical settings prior to
the war
but had been abandoned with the discovery of effective
antibiotics. It
would be revived again long after the war, when antibiotic
resistant
bacteria increased the need for very careful debridement.
Burns.
Burns were particularly common under the combat conditions seen by
the
Navy. Navy medical officers soon distinguished between deep burns,
usually inflicted by hot steam or burning fuel oil, and flash burns
inflicted by explosives.
Ordinary cotton clothing provided considerable protection from
flash
burns, and Navy regulations soon required sailors to wear
long-sleeved
shirts and pants even in the hot
tropics. Combat veterans went even
further, tying off the ends of their pants, wearing gloves, and
keeping
their jumper hoods over their heads while at battle stations.
Patients with extensive deep burns rarely had good outcomes. The combination of fluid loss from the burned tissues and infection of the large open wounds they produced was usually fatal. Modern techniques for treating burns were in their infancy in 1941 and made relatively little progress during the war. Like wounds, deep burns required debridement to remove dead tissue that was a source of infection. Unfortunately, this increased fluid loss through the burn and increased the risk of shock. The use of skin grafts as treatment for burns was not unknown, the first dermatomes for harvesting healthy skin having been introduced in the 1930s, but the present standard of care (thorough debridement followed by extensive skin grafting) was not widely accepted until the latter half of the 20th century.
Burns were treated with tannic acid solutions, a
method introduced in 1925. The tannic acid reduced pain and
patients
treated with tannic acid had better outcomes. It was thought that
the
tannic acid, by coagulating proteins in the burned flesh,
prevented
toxic compounds from entering the blood stream, and that the crust
it
formed over the burns helped prevent shock from fluid loss. It
also had
mild antiseptic properties. Tannic acid treatment was abandoned
late in
the war out of concerns that the tannic acid could enter the
bloodstream and produce serious liver damage. It was largely
replaced
by sulfa jellies, which did less damage to the burned tissues and
were
much more effective at fighting infection. Gentian violet was also
used
as an antiseptic on burns.
Anesthesia.
The first treatment given most casualties was an injection of
morphine
to ease suffering. American medics carried syrettes containing
half a
grain (32 mg) of the drug, which was usually enough to deaden pain
and
put the
casualty to sleep. Additional morphine could be administered at
the
battalion aid station if needed. Morphine was very effective, but
it
was also potentially addictive, and it aggravated shock by
depressing
body
functions. Local and regional anesthetics, such as epidurals, were
already in use when war broke out, and their use avoided some of
these
difficulties.
Milder analgesics included aspirin and phenacetin, the latter a forerunner of acetaminophen (Tylenol) that is no longer used today because of its potential to cause cancer.
Supplies of morphine were sometimes exhausted by heavy casualties among Western forces, forcing physicians to reserve the supply for the worst casualties. However, accounts of surgery without anesthesia are so numerous from Japanese veterans that they suggest a cavalier attitude towards the suffering of wounded soldiers and sailors. Werneth (2008) quotes one pilot at Coral Sea:
Watanabe-san, who was one of my men, had fragments in his face.... At that time there was no anesthetic, but right after someone was injured, it was okay to perform an operation because he was somewhat paralyzed due to shock. However, if the operation took a long time, it could be painful.
This was one of several Japanese Navy pilots interviewed by
Werneth who reported surgery without anesthesia.
Illness.
The same antibiotics that proved so useful against wound infection
were
also effective against a number of diseases. Sulfa was so
effective
against bacterial pneumonia that it was said to have "dethroned
the
captain of the men of death." However, none of the antibiotics
were
effective against viral infections such as influenza, viral
meningitis,
viral pneumonia, or yellow fever.
Nor were the new antibiotics useful against malaria, the scourge of troops
in
tropical and semitropical regions. The traditional preventive,
which
was
reasonably effective, was quinine.
This became unavailable to the Allies with the loss of Java, but atabrine became an
effective
alternative. The greatest difficulty was getting the troops to
take
their atabrine doses: The drug was extremely bitter, its dosing
was not
well established and overdoses produced very unpleasant symptoms,
including psychosis. The
drug tended to discolor the skin even at appropriate doses, and
the
rumor spread that it caused infertility (which was not the case.)
Following the Japanese surrender,
in late August 1945, Operation MASTIFF was mounted to drop over a
million doses of atabrine by parachute to prisoner of war camps.
Dengue was another tropical disease that put large numbers of troops out of commission. Like malaria, dengue was spread by mosquitoes, and mosquito control measures used to control malaria also helped control dengue. Unlike malaria, dengue was caused by a family of viruses. None of these built immunity against any of the others, so it was possible to get dengue more than once. The symptoms were high fever and excruciating pain in the bones and joints ("breakbone fever"), though the fatality rate was usually low.
Another scourge was scrub typhus, which was spread by mites
inhabiting scrub undergrowth. The carrier mites were also common
in the
kunai grass that often marked the best sites for airfields. The Allies learned
the hard way that New Guinea natives who regarded
certain areas as tapu, forbidden, were not just indulging
in superstition: The tapu areas were often havens for
mites. Untreated, the death
rate
from scrub could be as high as 40%. A vaccine was not available
until June 1945,
and it was not very effective, since the primitive bacteria
(rickettsia) responsible for the disease show considerable
antigenic
variability. None of the antibiotics of the time were effective
against
the disease, and the disease could be controlled only by
destroying the
mites that transmitted it. DDT
was less effective against mites than it was against insects, and
the
usual control measures were to burn off brush and kunai grass and
thus
deprive the
mites of their habitat and to require troops to wear clothing
impregnated with dimethylphthalate.
Dysentery was a common ailment on almost all battlefields. It was typically transmitted by flies and other insects that fed on both feces and the soldier's food supply. It could also be transmitted when fecal matter contaminated the water supply. Medical officers attempted to enforce strict field sanitation, but soldiers under fire who could not leave their foxholes had little alternative to simply tossing their wastes a short distance outside their holes. Water could be purified by boiling or addition of iodine or halazone tablets, which were included in the U.S. Army C ration. A minor scandal during the Peleliu battle was the use of inadequately cleaned oil drums to transport water, which made a number of troops ill.
Troops already ill with bacterial dysentery could be given fluids to replace losses from diarrhea, but otherwise the disease had to run its course. The antibiotics of the time (sulfanilamide and penicillin) were ineffective against the gram-negative bacteria that usually caused the disease. Amoebic dysentery was a more serious disease, sometimes causing abscesses in the liver or other internal organs. However, amoebic dysentery could be treated with the antimalarial drugs, quinine and atabrine.
A number of prisoner of war camps run by the Japanese experienced epidemics of diphtheria. This disease usually attacks the throat, and can kill either by closing the airway with swollen and dying tissue or by secreting a potent toxin that causes heart failure. Diphtheria could be treated with antitoxin and sulfa drugs, but neither was made available to the prisoners, and the fatality rate was high.
Another threat in prisoner of war camps was cholera, a particularly severe form of bacterial dysentery. One British prisoner on the Burma-Siam railroad described what it could do to weakened and overcrowded groups of men (Gilbert 1989):
I have just received news that 130
British soldiers in the camp cross the road died yesterday. The
cholera only hastened the end for these deathmasked men.
Dehydration,
in a black coat, is taking the victims painfully away.
Cholera was not just a threat to prisoners of war. 11 Army suffered severely from a cholera outbreak in central China in July of 1938. A Japanese medical officer described an outbreak in his unit in Burma (Tamayama and Nunneley 2000):
We came close to Ye-u and were resting under trees by the River Ye-u, when a non-commissioned officer started vomiting severely followed by violent purging of white liquid faeces every three or four minutes. His hands and feet became cold and wrinkled, and he was badly dehydrated. This was the dreaded outbreak of cholera.
The sick men were quarantined and heightened field sanitation
measures imposed, but the unit had only six bottles of Ringer's
solution for intravenous rehydration, and was forced to improvise
using
juice from palm fruit as a source of electrolytes. This worked
better
than the unit had any right to expect.
Heat exhaustion was a common problem in tropical zones. The adult human body cannot tolerate an internal temperature above 104 degrees Fahrenheit (40 degrees Centigrade) for any length of time, yet temperatures in some parts of the tropics reached 120 degrees or greater. The response of the body is to sweat to remove heat by evaporation, but in jungles where the air was already saturated with moisture, evaporation is slow and sweating becomes profuse. Troops who failed to drink enough water or to take salt tablets to replace salt lost in sweat risked serious heat illness. This was treated by rapidly cooling the patient by whatever means were available (typically an ice bath or, where ice was unavailable, swabbing with alcohol) and restoring fluids and electrolytes. An unanticipated consequence of fighting in tropical climates was the need for larger stretcher teams, since two men carrying a stretcher rapidly became exhausted in the heat.
Another jungle scourge was fungus infections of the skin,
universally known to the troops as "jungle rot" or "the crud."
Superficial fungus
infections were treated with a solution of potassium permanganate,
which was irritating to the skin and stained it purple, but was
effective at killing the fungus. Filipino guerrillas, lacking any
other medications, sometimes used picric acid from recovered
Japanese mines (a highly
dangerous activity) as an antiseptic to treat jungle ulcers.
Trench foot disabled many troops. It was the consequence of failing circulation in the feet. Infantry who laced their boots too tightly and soaked their feet in cold water or mud were most vulnerable, since cold contracted the small vessels in the feet and could trigger a downwards spiral. Sledge (1981) described his experience:
It was great to wash my feet, holding them up on an ammo box to let the sun shine on them while I wiggled my toes. Everybody got his feet clean and dry as soon as possible. Mine were extremely sore and red over the entire soles, almost to the point of bleeding. All of the normal friction ridges of the skin had sloughed off, and the soles were furrowed with deep, reddish grooves. But after drying them in the sun and putting on dry socks and boondockers, they soon felt better. Months passed, however, before the soles appeared normal again.
Sledge's was a mild case. In more severe cases of trench foot, the pain could be agonizing, and sometimes amputation was necessary due to gangrene.
Typhus was one of the dreaded diseases of wartime, often reaching epidemic levels among populations rendered susceptible by exhaustion, malnutrition, and poor hygiene. It caused upwards of six million deaths during the First World War and in the war's aftermath. The disease is transmitted by lice, and the best control measure available prior to 1938 was delousing. However, the Cox vaccine, a typhus vaccine grown in chicken embryos, virtually eliminated typhus as a threat to Allied troops, with just 11 soldiers out of a million in North Africa contracting the disease when an epidemic broke out in the civilian population. Civilian typhus control was accomplished largely with DDT administered with dust guns, which allowed the insecticide to be blown under civilian clothing without requiring the civilians to disrobe — a serious concern with Muslim women in the Mediterranean theater. The clothing actually made the treatment more effective by holding the insecticide close to the skin.
A sizable number of Marines stationed at Upolu developed symptoms of
filariasis, an infection by tiny roundworms
transmitted by mosquitoes. The disease normally required prolonged
exposure before the characteristic symptoms (swelling of the lower
extremities from blockage of the lymphatic system) became
apparent.
However, under the stress of combat, many of the infected Marines
showed symptoms severe enough to
require their return to the States. It was found that the symptoms
reversed themselves when the patients were returned to a temperate
climate. Prevention was by the same mosquito control measures
applicable for malaria.
Hookworm was a problem at Aitape. The eggs hatch in the soil and the young worms penetrate the skin and migrate to the intestines, where they suck blood voraciously. Prevention by avoiding contact with contaminated soil was the best control, but the worms could be expelled with treatments using thymol (oil of thyme) and magnesium salts.
Venereal disease was almost unknown among Allied troops in the South
and Southwest
Pacific, other than those stationed in Australia. It became a more
serious
problem when American troops returned to the Philippines, and it
was a very serious problem among troops stationed in India, where the rate among
British troops was up to 49.4 cases per thousand by 1943. It could
be
prevented by supplying troops with condoms and by allowing troops
the
use of brothels that were discreetly supervised by medical
officers —
a controversial measure among the Allies, but an accepted institution
in the Japanese Army. Infections with gonorrhea could be treated
with sulfa drugs, but sulfa was ineffective against syphilis,
whose
cure had to await the availability of penicillin.
Almost all armies and navies that fought in the Pacific held
periodic inspections of their men to look for signs of venereal
disease. These were known informally as "short-arm inspections" in
the
English-speaking armies. In
the Japanese armed forces, contracting a venereal disease through
carelessness was considered a serious offense and could result in
reduction in rank. Repeat offenders could be sentenced to
confinement
but were sometimes punished less formally, by being beaten while
in
hospital for the condition. Such severe penalties were meant to
prevent
loss of manpower due to venereal disease, but they gave the
troops a strong incentive to conceal infections. For this
reason
the Western armies generally avoided formal punishment except for
repeat offenders.
Malnutrition. Forces cut
off
from their supply chain
risked
malnutrition and starvation. Victims of malnutrition included the
Americans in Bataan, prisoners
of
war held by the Japanese, and
Japanese garrisons bypassed by the Allied counteroffensive, such
as 17 and 18 Armies.
Shortages of vitamin A in the diet led to night blindness, while shortages of vitamin C caused scurvy. Scurvy is characterized by anemia and spongy gums. Deficiency of thiamine (Vitamin B1) caused beriberi, which was characterized by neuropathy and damage to the heart. Lack of niacin (Vitamin B3) produced pellagra, characterized by dermatitis, diarrhea, and dementia. Almost all vitamin deficiencies slowed the healing of even minor wounds. The only treatment was administration of the missing vitamins.
The rations consumed by the Japanese Army were based on polished
rice and were so poor in thiamine
that
Japanese troops sometimes showed signs of beriberi even in
garrison.
Any breakdown in logistics rapidly caused large numbers of
Japanese
troops to come down with the full-blown illness. This was evident
at Guadalcanal,
where large numbers of Japanese were encountered during their
retreat
who continued to wield a rifle
even though they could no longer stand
due to neuropathy in their lower limbs.
Young men engaged in heavy combat needed to consume as much as 3500 calories per day to maintain body mass. Any less meant weight loss, which could go only so far before the body's fat reserves were exhausted and muscle began to waste. This included the heart muscle, and prolonged starvation could produce irreversible heart damage even if the victim eventually had his source of calories restored. Hundreds of Allied prisoners of war who lived through the surrender died prematurely after the war from this lingering effect of their ordeal.
Some starving soldiers died of heart failure a few days after
being
rescued and resuming eating. This was often attributed to an
inability
to digest solid food, but it may also have been due to sudden
uptake of
phosphate by the body's cells with the restoration of carbohydrate
sources of energy, which disturbed their entire electrolyte
balance.
Starved soldiers were kept on controlled diets in which their
intake of
calories was gradually increased, which helped their bodies slowly
adapt without severe electrolyte imbalances.
Frostbite. This was a serious problem in the Aleutians campaign, among airmen operating at high altitude, and — incredibly — among troops in New Guinea, who discovered that freezing temperatures were possible at night in the Owen Stanley Mountains. Treatment consisted of gently warming the frozen tissues to avoid damage that might lead to gangrene. The U.S. Air Force responded with electrically heated flight suits and improved hatches for gun ports.
Snakebite. Okinawa is the habitat of the habu, a venomous snake of the pit viper family, related to the rattlesnake of North America. Prior to the Okinawa campaign, Service Force, Pacific Fleet stockpiled a supply of antivenin from the Indian snakebite laboratory at Calcutta to treat snakebite victims. As it turned out, the threat was exaggerated, and there were very few snakebite victims.
Triage. One wrenching aspect of military medicine is the need for triage to determine where to use limited medical resources when these were overwhelmed by the numbers of sick or injured persons. Though improvements in medical care greatly reduced the need for triage in the Pacific War compared with previous conflicts, there were still situations in which medical personnel had to make painful choices of which patients to treat first.
Triage sorted patients into the non-urgent, who could wait some
hours for
treatment without serious risk of death or complications; urgent,
who
were at risk of serious complications if not treated within a few
hours; emergent, who were in immediate peril of death or serious
complications, but who had a good chance of survival with prompt
treatment; and the moribund, who had a poor chance of survival
even
with immediate treatment. When medical facilities were flooded
with
patients, non-urgent cases went to the back of the line, but so
did the
moribund, since limited resources were better used on patients who
were
more likely to be saved.
Under the Geneva and Hague Conventions, medical personnel were granted complete immunity so long as they did not engage in any military activity. Medical personnel were expected to wear a white brassard (armband) bearing the Red Cross so that they could be identified from a distance. The prohibition against engaging in military activity meant that Allied medics were generally unarmed early in the Pacific War.
German troops (except the SS) usually respected the Red Cross, lifting their fire when medics were evacuating casualties, as did the western Allies. Medics serving in Europe painted a large white field with a Red Cross on their helmets to make themselves stand out more clearly on the battlefield, a clear indication that they believed the Red Cross was being respected by their enemies. This was not the situation in the Pacific War. Although the Japanese Navy largely honored the hospital ship convention, the Japanese Army repeatedly bombed Allied hospitals, murdered doctors and patients in hospitals they overran, and seemed to consider the Red Cross a convenient aiming point on the battlefield. Five of every 100 medics serving on Attu was killed while treating or moving the wounded. The failure of the Japanese to respect the Red Cross convention led the Allies to give their medics "defensive arms" such as pistols (which the Allies claimed were not prohibited under the Conventions if used only to protect medics and their patients), and medics stopped wearing the Red Cross brassard. Bandages were dyed green since white bandages were yet another convenient aiming point for Japanese riflemen.
Allied intelligence claimed in 1944 that Japanese medics
routinely carried arms and were used as replacements for combat
units. American commanders in the Pacific were deeply suspicious
of the heavy hospital
ship
traffic under the Japanese flag, a suspicion that was confirmed by
decoded Japanese messages
showing the Japanese were attempting to use the hospital ships to
transport troops. However, the great secrecy surrounding
cryptanalysis meant that the Allied commanders could neither act
on nor publicly disclose this violation, which did not come to
light until the 1990s (Weinberg 1994).
U.S. Military Medicine. In peacetime, U.S. Army physicians were regular officers and could theoretically be line commanders. Some, like Leonard Wood, who rose to the post of Army Chief of Staff (the senior officer of the Army), ceased to be doctors in all but title. Others struck various compromises between the profession of medicine and the profession of arms. The character of Colonel Sherman Potter in the popular television series, M*A*S*H, was not an outrageous Hollywood fabrication. By contrast, dentists and veterinarians were all reserve officers and did not have command authority. In emergency situations, dentists were often called on to back up the limited supply of physicians, while veterinarians also acted as sanitation officers, a role they had acquired as slaughterhouse inspectors.
Peacetime Navy physicians were also regular
officers, but they were not line officers and commanded no unit.
However, they were tightly integrated socially with the other
officers
on board ship,
who
regarded them as the valuable specialists they were. Because Navy
physicians also served the Marine
Corps, they were often posted to foreign shore stations,
where they
had some opportunity to gain experience with the kinds of exotic
diseases and difficult conditions that would later characterize
combat
medicine in the Pacific War.
In peacetime, Army and Navy physicians were rigorously selected and then trained in military medicine at the Army or Navy Medical School. Many then received postgraduate training at general hospitals. Enlisted corpsmen often remained in that specialty their entire career, and Navy corpsmen on small ships were the only medical authority on board. They often developed a very high degree of competence: During the war, there were at least two cases of a submarine sailor deep in enemy waters having his appendix removed by a Navy corpsman working from a textbook. Both survived. In addition to corpsmen, all Navy officers were trained in first aid.
Each Western division
included a medical battalion
in
its TO&E,
along with detachments at lower echelons. This permitted a
hierarchy of
medical care, with first aid rendered by medics (Army) or Navy
corpsmen
(Marines) assigned to
individual companies at the
front
line.
Casualties were then moved to a battalion
aid station a few hundred yards behind
the line, where there was one or more physicians on duty. The
physician
here evaluated the injury and, if it was serious enough, sent the
wounded man on to a clearing station, a kind of mobile clinic
where
more sophisticated emergency treatment was given to stabilize his
condition. Once his
condition was stabilized enough for further transport, the
seriously
wounded patient was evacuated
to a field or surgical hospital. From here the most serious
casualties
were evacuated to evacuation hospitals, normally situated 12 to 30
miles (30 to 50 km) behind the front line.
The very worst casualties were then sent by air transport or
hospital ship to general
hospitals to the rear of the combat zone. These general hospitals
were
equipped to provide the most modern and extensive medical care.
Later
in the war, convalescent hospitals were established for patients
whose
wounds had healed but who were not yet ready for the rigors of
combat.
Casualties were not evacuated to the United States from the
Southwest
Pacific or South Pacific unless they were expected to require more
than
90 days to recover (an even longer limit was adopted in other
theaters); nevertheless, some 518,000 Army patients arrived in the
United States by hospital ship, and another 121,400 by air
transport,
from all theaters during the war.
Army and Navy doctors complained that the "mobile field hospitals" were not actually very mobile. The Seabees were supposed to set them up but often had other priorities, leaving the medical staff themselves to do much of the construction (quoted by Cowdrey 1994):
The brain surgeon put on the roof, the dental officer installed the ventilators, the psychiatrist put up the side walls, the eye man put in the windows, one surgeon laid the decks, and another surgeon and the skin man put in the floor beams while the obstetrician dug the holes and put in the footings for the foundations.
Mobile surgical hospitals were first standardized in the
Southwest Pacific in 1942, with facilities for 25 patients.
Air evacuation of casualties was an important development in the
Second World War. Three times as many casualties were evacuated
from Guadalcanal by air
as by sea.
Patients evacuated by air had to endure less rough handling and
had
better outcomes. In theory, air transports marked
with the
Red Cross
were as immune to attack as hospital ships, but it was convenient
to
evacuate casualties in the same transports that brought in
military
supplies,
precluding such markings. Furthermore, a Red Cross on an aircraft
was likely to be mistaken for the Japanese hinomaru and
result in a friendly fire
incident. Allied control of the air was thorough enough
that few were lost to enemy action.
Total Army hospital admissions were 8.9 million in the United States and 5.1 overseas, of which the vast majority were clearly not combat-related.
Commonwealth military medicine resembled that of the United States, except that doctors were subject to assignment where needed in Britain, rather than being recruited on a voluntary basis. Penicillin was originally a British discovery and was brought to America for production largely because Britain was subject to destructive air raids.Japanese military medicine trailed well behind Allied medicine. While the best Japanese physicians were as good as any in the world, they were fewer in number due to Japan's relatively recent modernization, and the chronic Japanese deficiencies in logistics meant that medical supplies were often in very short supply at the front lines. A Japanese division included three field hospitals in its TO&E, each with 45 ambulances, but in most divisions these existed only on paper. Sometimes the shortage of medical personnel was made up by conscripting whole schools of teenage girls, who received little training before being shipped to the combat areas. Japanese physicians had no access to the newer drugs, such as penicillin, that were developed in the Allied countries during the war. Nor were they provided with the freeze-dried plasma that became a standard medical item in Western armies, instead making use of lactated Ringer's solution to maintain circulation following blood loss. When Japanese wounded could not be evacuated, they were encouraged to commit suicide rather than be taken prisoner. Those unable to kill themselves were killed by their doctors, often by lethal injection. This reflected the cavalier attitude towards human life manifest throughout the Japanese military.
Such poor Japanese military medicine was a relatively recent
development. Foreign observers of the Russo-Japanese War
considered
Japanese military medicine to be the best in the world,
particularly in
preventative hygiene, and of the 9,862 wounded Japanese soldiers
admitted to hospitals by 1 August 1904, only 34 died. It seems
unlikely
that the poor performance of the Japanese Army medical services in
the
Pacific War can be explained by lack of physicians or logistical
difficulties alone. It was likely part of the "sea change" in the
Japanese Army in the 1930s, when the Army was transformed from a
force
notable for its correct behavior in earlier conflicts to a force
notable for its extreme brutality.
Chinese military
medicine. The Chinese Army was in the worst shape of
all.
There were at most a few thousand doctors for an army of millions,
and
medical supplies were almost nonexistent.Though a medical college
was
established as early as 1912, becoming Peking Army Medical College
in
1926, most Chinese Army formations lacked any medical officers.
Large
numbers of
non-physician medical officers and nurses were given rudimentary
training in first aid, which probably saved many lives, but fell
far
short of the need. Casualties tended to be abandoned where they
fell,
except for a lucky few treated by medical missionaries. Even during the
Battle of Shanghai in 1937,
where the best hospitals in China were close by, the survival rate
for wounded Chinese soldiers was only 50%.
The Chinese Red Cross, under Dr. R.K.S. Lim, tried to assist, and by the late 1930s it was wholly devoted to military medicine. The Chinese Boy Scouts gave valuable service and were praised for their reliability and intelligence. Their ranks included a significant number of young men over the age of twenty, who did such things as driving medical vehicles. Many came from the upper middle class, which otherwise had a poor record of supporting the war effort with individual service and sacrifice.
Nevertheless, medical training continued to be given a low priority. In 1943, of nearly 6000 candidates for admission to National Central University, 31% chose engineering, 25% law, 12% each education and agriculture, 10% humanities, and only 5% each science and medicine. This reflected Chinese perceptions on which fields were most important for modernizing China and repulsing the Japanese invaders.
By spring 1938, most units were equipped with stretchers and
stretcher-bearers.
That this was considered a significant accomplishment speaks
volumes.
In the Hsuchow campaign, it
took
from one to three days for a casualty to be transported from the
front
to the city. Here the casualty received first aid and, if he was
lucky,
a bed. Surgery required an overnight train ride to to Chengchow. The trains went
out
nightly, were equipped with rush mats and some food and water, and
had
attendants and a doctor or two on board. This was considered a
major
improvement over previous practice. More serious cases went to Hankow. Some 20,000 casualties
were
processed through this system in the first half of April 1938,
during
the Battle of Taierhchuang, and few had serious wounds of the
chest,
thorax, or abdomen, suggesting that few of those so injured had
survived long enough to reach the rear areas. A Dutch observer
noted that about half of all wounded Kuomintang soldiers died of
their wounds.
The lack of even basic medical care close to the front meant that
the evacuation lines were flooded with slightly wounded men who,
in the
Western armies, would have been quickly treated and returned to
duty.
Another consequence was that a disproportionate number of
casualties
had superficial wounds to the hands or feet, suggesting that they
had
been self-inflicted as a way to escape to the rear areas.
An American observer, Captain Frank Dorn, visited a military hospital in Nanchang (Hsiung and Levine 1992):
None of the supposed eleven doctors on duty was doing anything, and the nurses and orderlies were virtually untrained. Wounded soldiers who had arrived in the hospital two or three days earlier had not even been washed or had their bandages changed. Dorn summed up his impressions with the withering comment that "the so-called care of the wounded in the 90th Military Base Hospital was deplorable.... the manifest ignorance of those in charge was not even tempered with any sign of kindness to the sick. Nurses and orderlies seem to view the men in their care with a completely callous disregard for their suffering."
Dorn had a notoriously sharp tongue when writing about all things
Chinese, but there can be little doubt that conditions in the
Chinese
military medical system were deplorable by Western standards.
Morphine
to ease suffering was nonexistent and even bandages were in such
short
supply that casualties often did not have their bandages changed
at all
during the three or four days it took to reach a rear-area
hospital.
Dorn also reported that victims of chemical
attack
were present at Nanchang. This was a challenge against which China
had
neither any defense nor any means of retaliation.
Illness was rife in the Chinese Army, where a dysentery rate of
10%
was the norm and malaria was so common (afflicting up to 80% of
troops)
that it received no more treatment than a cold. In 1936, 10% of
the soldiers became ill, and perhaps 5% of these died.
However, there is no question but that Chinese medical medicine
improved considerably during the first four years of the second
Sino-Japanese War, from virtually nonexistent to merely tragically
inadequate. It broke down every time the Japanese made a rapid
advance,
leaving countless seriously wounded to die where they fell.
References
"Handbook of Japanese Military Forces" (1944-9-15)
Hearing (2004; accessed 2009-10-5)
"Lymphatic
Filariasis" (accessed 2012-9-14)
Office
of
Medical History (accessed 2009-9-26)
Paul (2008; accessed 2009-9-26)
Steinert (2000; accessed 2009-9-26)
Time (1938-11-28; accessed 2010-1-21)
Zoobiotic.org
(accessed 2011-6-18)
The Pacific War Online Encyclopedia © 2008-2009, 2011-2015 by Kent G. Budge. Index